Navigating Ontario’s mental healthcare system can be frustrating.
Every day, 200 Canadians grapple with the harrowing decision to attempt suicide. S@Y News reporter Jamila Apolinario dives into the pressing issue of mental health in Ontario, speaking with individuals diagnosed with mental health disorders and experts in the field.

“Imagine you have severe depression. And you’re alone,” says “John,” an international student. He asked for his identity to be protected. “Every time I woke up it’s like it’s like a atomic bomb to my head. Like I’m exploding every time I woke up I’m having some panic attacks.”
“I’m fighting this battle all alone.”
“They’re just doing their jobs but there’s no sympathy that’s why I never want to go back to hospital so I’m doing this all alone. I’m fighting this battle all alone,” John said. He also says that he now hesitates to seek medical support from professionals due to previous experiences.
Statistics Canada reports that annually, more than 5 million Canadians are diagnosed with mental health disorders , which is equivalent to a third of Ontario’s population.
“I tried to seek help…”

Augusto Abilio had a similar situation as John. Abilio mentions that he frequently faces rejection when attempting to access Ontario’s mental healthcare system, and he indicates that he only receives treatment during life-threatening situations.
“I tried to seek help at CAMH. But over there they say that I was not in a moment of crisis as deeply needed for me to be accepted,” says Abilio, who spent a brief period hospitalized for treatment of a mental health condition.
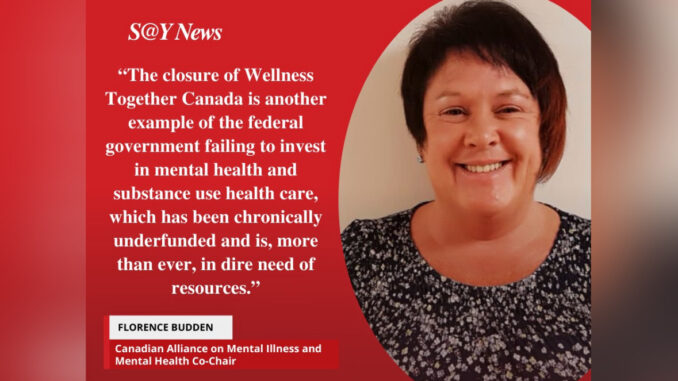
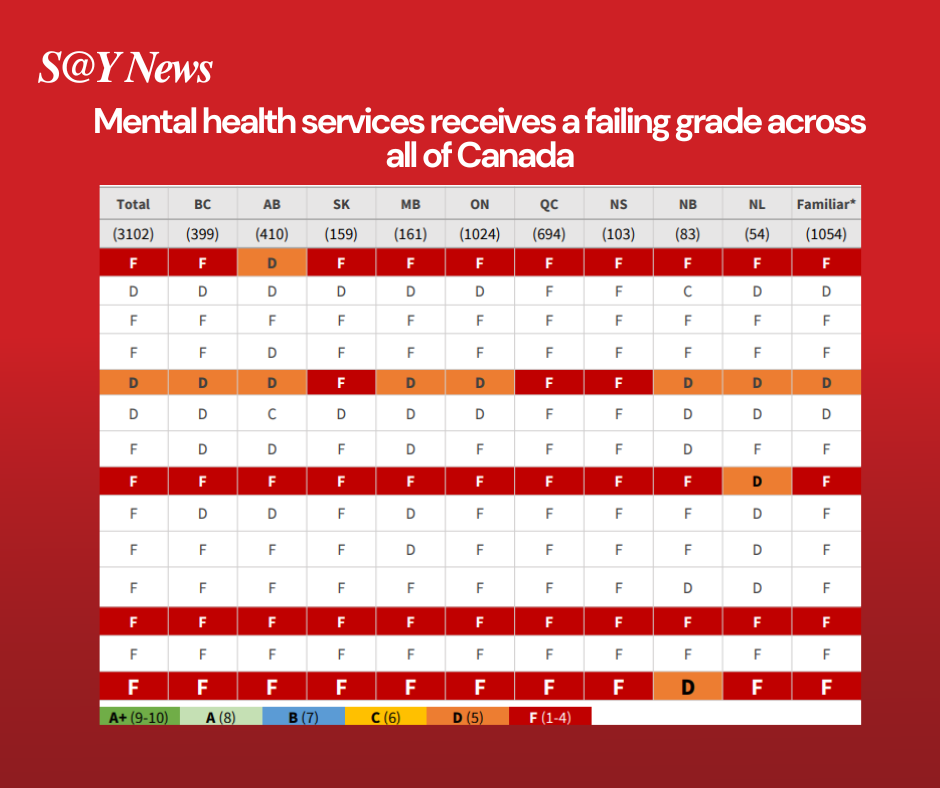
A survey conducted by the Canadian Alliance on Mental Illness and Mental Health (CAMIMH) reveals that Canadians have given mental health services across the country failing grades, with the federal and provincial governments receiving an ‘F‘ for mental health services and a ‘D‘ for substance use services.
Florence Budden, co-Chair of CAMIMH, has expressed criticism towards the federal government’s decision to halt funding and shut down the Wellness Together Canada portal. This platform, which was launched amid the pandemic, aimed to offer accessible mental health support to the public.
Statistics Canada indicates that while there has been a decline in the number of individuals seeking mental health support, these numbers still exceed the figures recorded before the lockdown.
“Not Aware that they have mental issues”

“Most of the time, people who are dealing with mental health issues are not aware that they have mental health issues, and that they’re also denying that they have mental issues for various reasons,” says Liezl Sebial, a social work professional. She also points out that one of the challenges individuals encounter when dealing with mental health disorders is having the will to seek help.
“There’s a lot of pressure in our youth now-a-days, with social media, with things that are being exposed,” Sebial said. “It’s really important that we provide them with the services because they’re developing, they’re young adults, they’re not really fully adults, but they’re not children anymore.” she added.
According to CAMH, teenagers and young adults have higher rates of mental illness and substance use disorders, with 39% of Ontario high-school students experiencing moderate-to-serious psychological distress. Men also show higher rates of substance use disorders while women have higher rates of mood and anxiety disorders. Furthermore, there’s a correlation between mental and physical health as individuals with chronic physical conditions are more prone to mood disorders, and vice versa.
“The Stigma”
“In the hospital, they [hospital staff] are always surprised because it was a group of people with a lot of men. And they were surprised because usually men don’t tend to seek for help as women because there is a cultural aspect to that,” Abilio said. He also explained that he comes from a Latin-American culture where they are forced to accept how they feel.
Sebial says that culture plays a big role on how people seek help and view the stigma of mental health. “Because for some, it’s shameful. It’s embarrassing for a family member in that particular culture to admit someone in [their] family has mental health issues,” she added.
“My life, my life is my family. And now… in just a snap. It’s all gone,” John said
In a 2019 Ipsos survey, three quarters of Canadians expressed hesitance or outright refusal to disclose a mental illness to an employer or co-worker, citing concerns about stigma, fear of being treated differently, and apprehension about negative consequences. That’s despite 76% indicating they would be comfortable and supportive of a colleague with a mental illness.
Mental Health and Addiction
“I had some attempt of harming myself in a permanent way. And two years ago, I had my my first real attempt. And that was the time that I was [taken] to CAMH and stayed there for a couple of weeks,” Abilio said.
According to StatsCan, more than 200 Canadians attempt suicide everyday, and about 12 of them died each day.

“The mental health crisis is a multifaceted issue. And I think that we’re seeing an increase in mental health disorders in general globally,” says Ari Daniel, harm reduction advocate. Daniel is the host of the podcast Addicts in the Dark. “There are many factors contributing to the crisis, and societal pressure, economic instability is a big one right now. Trauma, genetic predispositions, and inadequate access to mental health services.”
“Before I’m afraid to go to hospital because of the trauma” John said. He also mentioned that besides trauma, financial worries are currently the primary concern. “I’m not taking medications right now because it’s too expensive for like antidepressants. Sleeping pills I used to have that, but not right now.”
“It’s really important that we take care of our mental health because it’s something that we don’t see or not physically see,” says Sebial.
Daniel says that individuals facing mental health disorders may resort to substance use as a means of self-medication and dealing with symptoms, potentially leading to addiction. “People may cope with addiction instead of seeking help for a variety of reasons,” he added.
“It’s very common for people to turn to drugs, especially if drugs are readily available, or that’s the only option that’s available to them at that time,” Sebial said.
Daniel argues that attributing the failure of Canada’s mental healthcare system to a single entity is overly simplistic, as the issue is complex and multifaceted.
“So don’t lose hope. Keep going and think that things are going to be better. They’re not going to be as dark as they look right now,” Abilio said.
Both the provincial and federal governments acknowledge the necessity for new facilities and additional resources. The Ford government recently unveiled a $1.6-billion investment for the construction of two new buildings at the Centre for Addiction and Mental Health (CAMH) in Toronto. The federal government has allocated $3.7 billion to address the healthcare needs of provinces.




Be the first to comment